The Psoas Major And The Urinary Bladder
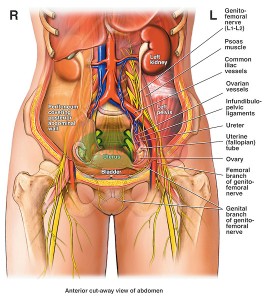
There is a relationship between the psoas major muscle and the urinary bladder even though they are not literally touching.
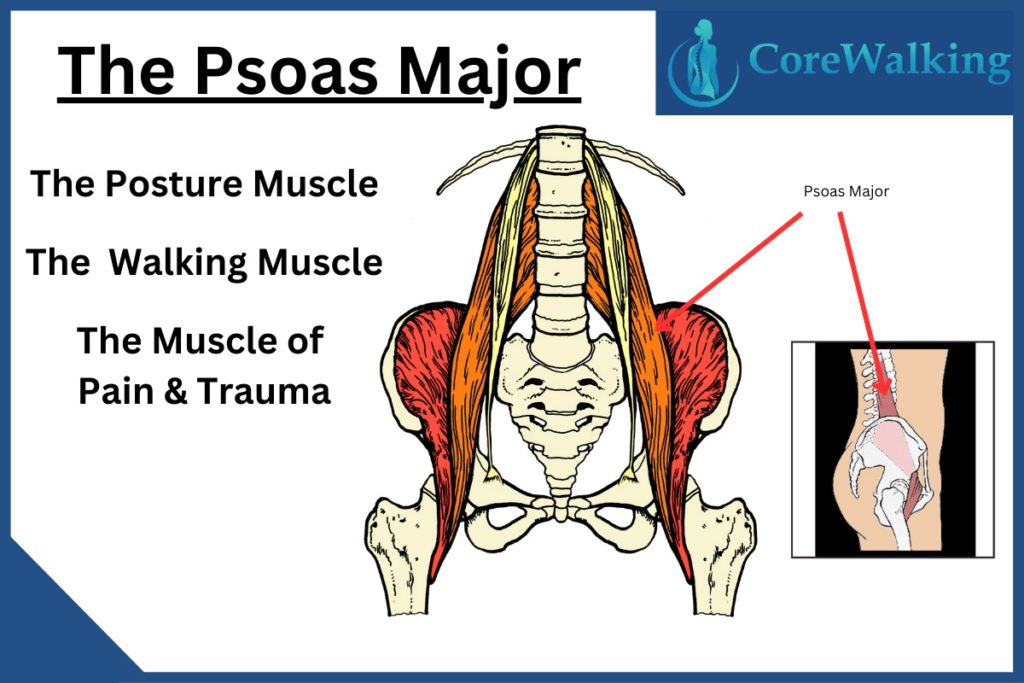
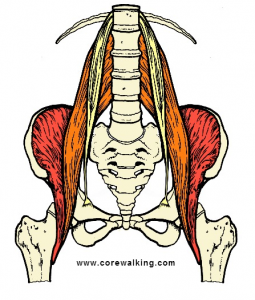
The psoas major is a muscle that is simply not on the radar of far too many people.
It is one of the most important muscles in the body and is one of only three muscles connecting the legs to the spine (piriformis and gluteus maximus are the others).
The psoas is the muscle of walking, and standing and most importantly for this post, it is the muscle of pain and trauma.
And a tight psoas, for whatever reason that it is tight, can interrupt the proper functioning of the urinary bladder while we sleep.
I have had the good fortune to work with a number of doctors with back pain over the years and I have been able to help many of them with my walking program and retraining their basic movement patterns to better serve their spine, pelvis, and whatever else was ailing them.
My rap is pretty basic—there is a design to the way the body is supposed to work and I try my best to explain in either anatomical or lay terms how that design can help them.
Many years ago after the second or third Psoas Release Party! workshop that I offered (which remains my favorite and most popular offering) I got an email from an attendee who reported that although she didn’t come to the workshop for urinary bladder related issues, after an hour and a half of concentrated release work she slept through the night without getting up to pee four or five times for the first time in a decade.
Obviously, this blew my mind at the time because, to be honest, I was swimming in uncharted territory myself, learning on the fly about this mysterious and profound muscle.
It’s All About the Psoas
It didn’t take a big leap in my imagination to think that a short tight psoas could disturb the urinary bladder and create an environment that would make someone pee repeatedly through the night.
So last week when I worked with a doctor who specializes in urinary bladder issues I went a step too far in saying that a tight psoas could press against the bladder when sleeping to cause someone to urinate multiple times over the course of the night.
She looked at me in a not-very kindly way and said, “Well you just lost me there because the psoas is about three inches away from the urinary bladder.”
I did my best to recover but thankfully this happened at the tail end of the session and I was able to slink away to look at my anatomy texts, which along with Google is where I do most of my learning.
Sure enough, the urinary bladder and psoas live in different counties, though all anatomy pictures show the same size urinary bladder which doesn’t account for the amount of fluid in them and long happy psoas muscles.
 For me, the idea that the psoas and urinary issues are connected is because a tight or traumatized psoas can’t sit back into the bowl of the pelvis and ends up closer to the bladder than a happy psoas might.
For me, the idea that the psoas and urinary issues are connected is because a tight or traumatized psoas can’t sit back into the bowl of the pelvis and ends up closer to the bladder than a happy psoas might.
Plus the tight miserable psoas might push the abdominal contents into the urinary bladder.
Finally, I think sleep position and the psoas can mess with the urinary bladder depending on how we are situated.
My goal is to get people to stop hiking one knee higher than the other which I think can affect our need to pee.
I know the doc was right about the literal anatomy of the psoas and urinary bladder but I have seen the effect of release work and sleep position on many clients.
When I offer my advice I am happy to hear back if it worked—and it doesn’t always.
I am also happy to be wrong about something because that is often when I do my best learning.
And in the eight years, since that first woman mentioned an ease in nighttime peeing, I have heard the same thing from many many clients.
Most importantly for the pure joy that I get from what I do, I love that it all remains something of a mystery, like the psoas itself.