What is degenerative disc disease?
There are several diagnoses out there that befuddle me, degenerate disc disease being one of them.
The main reason for my consternation is that it is not a disease—it is considered to be a natural part of the aging process.
While I highly value MRIs and their ability to see microscopically into our bones and joints, they have a downside.
If someone aged fifty goes for an MRI that reveals degenerative disc disease, there is no baseline to compare this to.
If that person had had an MRI ten years earlier that showed a spine without degenerative disc disease I would put much more stock into the diagnosis at fifty.
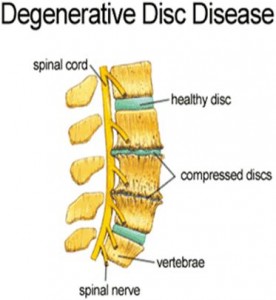
The spine is made up of 25 vertebras, give or take one or two. In between each vertebra is a fluid-filled disc that acts as a shock absorber providing a cushion between each of the bones.
The discs are made of a strong outer shell with a softer center.
There are many ways for these intervertebral discs to suffer. A bulging disc occurs when pressure from the vertebrae causes the disc to bulge out past the normal range of the spinal column.
A herniation is when the bulge goes to the next level. Both of these issues can be a major problem if they impinge on a nearby nerve.
Where spinal stenosis is degeneration and narrowing of the bony spine, degenerative disc disease is when the discs between the vertebrae begin to wither.
Degenerative disc disease tends to happen most frequently in the lumbar (lower) and cervical (upper) spine. I think the thoracic spine which is also home to the rib cage is spared because of the ribs.
The cartilage and muscles separating each rib also provide a certain amount of support to the discs in that area.
So while I take issue with calling a natural part of the aging process a disease, I also have a problem calling attention to it without offering a concrete means of alleviation and most often there isn’t much offered.
There is no stopping the march of time but we can slow it down a bunch.
The spine’s role as a shock absorber is one of its primary functions.
To absorb shock successfully it has to be properly aligned. This is rarely the case and our spines can take an alignment beating in so many different places.
Forward head posture messes with the cervical spine. Excessive kyphosis (rounding of the upper back) puts undue stress on the thoracic spine.
Last week I wrote about the thoracolumbar joint and its insecure place in the chain, and finally, a misaligned pelvis messes with the equally important lumbosacral joint.
While the aging process affects our spine, postural misalignments plague the spine in an equally profound way which can and do lead to degenerative disc disease.
Although you can’t mitigate the fact that we are essentially drying out and desiccating as we age which by its nature leads to degeneration, there are two main factors that we have control over in the search for a vital and pain free adulthood.
1. Skeletal alignment
2. Muscle tone
If we stand and move well we reduce a great deal of stress that it otherwise placed on the joints of the body.
Good posture and movement patterns allow for a poised skeletal system that will handle the vagaries of aging much better than the alternative.
It is better to be strong then weak. I don’t mean super human strength—just composed muscle tone that supports the skeleton but especially the spine.
I often refer to what I call the holy trinity of muscle groups—the inner thighs, the pelvic floor and the abdominals—as our most important maintenance system for the psoas muscle but you can substitute the spine for the psoas.
Developing balanced tone in these muscles can provide you with the best ammunition in the war against aging and the somewhat inevitable arrival of degenerative disc disease.
***